Comprehension of the anatomic deformities is central to understanding the principles
of their surgical repair. The following section briefly describes the anatomic abnormalities
in the patient with cleft lip and palate (CLP) by discussing the muscular, neurovascular,
structural, and nasal deformities.
Failure of the muscles to meet their counterparts during embryonic development leads
to the functional abnormalities of clefts of the lip and palate. The nonfunctional
substitute attachments lead to atrophy of the muscle units or maladaptive accommodation.
Modern cleft lip and palate surgical repair involves detachment of musculature from
atypical locations and realignment in a more anatomically functional position.
Cleft lip
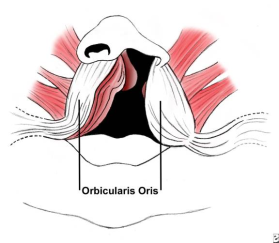
The orbicularis oris muscle is the primary muscle of the lip and can be divided
functionally and anatomically into 2 parts (see the image below). The deep component,
in concert with other oropharyngeal muscles, works in swallowing and serves as a
sphincter. The superficial component is a muscle of facial expression and inserts
into the anterior nasal spine, sill, alar base, and skin to form the philtral ridges.
In a complete cleft lip (CL), the deep fibers of the orbicularis oris muscle are
interrupted by the cleft and end on either side of the defect instead of making
their way around the mouth. In addition, the superficial component of the orbicularis
oris turns upward, along the margins of the cleft and ends beneath the ala or columella.[4]
Incomplete cleft lip behaves in a similar manner, except when the cleft is less
than two thirds of the height of the lip.[4] In this case, the fibers of the muscle
run along the margins of the cleft, then change direction and run horizontally over
the top of the cleft. These muscle fibers are interspersed with connective tissue.
The blood vessels parallel the course of the muscle fibers and run along the margins
of the cleft toward the columella or alar base, where they form anastomoses with
nearby vessels.
In the bilateral deformity, the anatomic characteristics are determined by the degree
of completeness of the cleft and its symmetry. The cleft may involve the primary
palate alone or in conjunction with the secondary palate. Although the prolabium
varies in size, it is usually retracted and lacks muscle fibers. In addition, the
columella is absent and the prolabium appears attached to the top of the nose in
some cases. The size and position of the premaxilla vary and effectively can be
excluded with a collapse of the alveolar arch.
The extent of nasal deformity associated with cleft lip varies from patient to patient,
although it has a characteristic appearance, with the following features:
- Deflection of the nasal tip towards the noncleft side
- Retroplacement of the cleft alar cartilage dome
-
Obtuse angle between the medial and lateral crura of the lower lateral cartilage
on the cleft side
- Buckling of the ala on the cleft side
-
Absence of the alar-facial groove on the cleft side and attachment of the ala to
the face at an obtuse angle
- Apparent or real bony deficiency of the maxilla on the cleft side
- Larger nares on the cleft side
-
Shorter columella on the cleft side, positioning the entire columella at a slant
toward the noncleft side
- Inferior displacement of the medial crus within the columella
-
Dislocation of the caudal portion of the septum to the noncleft side from the nasal
spine
- Downward rotation of the alar cartilage on the cleft side
-
Bilateral deformity in which the nasal tip appears large, flat, and bifid, because
both alae are rotated downward and spread apart
Cleft Palate
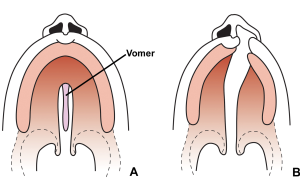
The incisive foramen is the key landmark in the bony palate (see the image below).
The premaxilla lies anterior to the incisive foramen and includes the 2 premaxillary
bones: the alveolus and the incisors.
The soft-tissue structures in the primary palate include the nasal tip and the upper
central lip. The size, composition, and configuration of the premaxilla can vary
from full development with the complement of teeth (4 primary and 4 secondary) to
underdevelopment with only 2 incisors. If the premaxilla is unrestrained in the
intrauterine and neonatal period it can protrude from the arch; the maxillary arches
may then collapse and potentially exclude the premaxilla from the arch.
Posterior to the incisive foramen lies the secondary palate, comprising the hard
palate and soft palate. The hard palate forms from the palatine processes of the
maxilla anteriorly and the palatine bones posteriorly. Posterior to the bony hard
palate lies the soft palate.
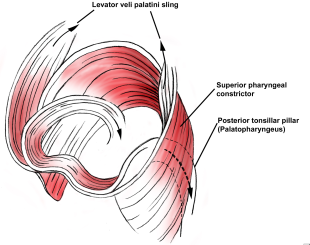
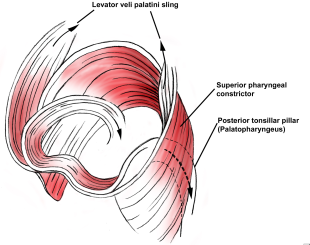
The soft palate plays an important role in speech and swallowing. Paired muscle
on both sides of the midline (see the following image) form the musculature of the
soft palate. The levator veli palatini is the most important muscle for the production
of speech and velopharyngeal competence. The paired muscles of the soft palate function
as a sling from their origin at the undersurface of the temporal bone to their aponeurosis
across the midline, as they elevate the soft palate toward the posterior pharyngeal
wall.
The palatopharyngeus further supplements the posterior movement of the soft palate.
Contraction of the superior pharyngeal constrictor contributes to closure of the
velopharyngeal opening at the lateral and posterior pharyngeal wall. The primary
function of the tensor veli palatini is to dilate the eustachian tube and to maintain
its integrity. The uvular muscle is thought to have a minimal contribution to normal
speech.
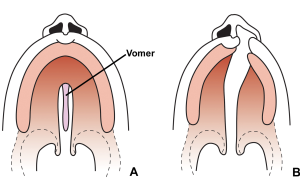
Clefts of the palate (CPs) are associated with bony, as well as soft-tissue, abnormalities.
Clefts of the secondary palate may be isolated or associated with clefts of the
primary palate. Although clefts of the secondary palate are midline defects (see
the image below), those involving the primary palate are usually asymmetric, with
the vomer attached to the noncleft side. The dental arch on the noncleft side usually
splays outward due to the lack of restraining force from the lip, and the palate
is foreshortened in the anteroposterior direction. In the case of complete bilateral
clefts, the entire premaxilla protrudes from the adjacent alveolar ridges. Because
of the collapse of the palatine shelves posterior to the premaxilla and its possible
rotation, the premaxilla is prevented from rejoining the arch and is left attached
solely to the vomer.
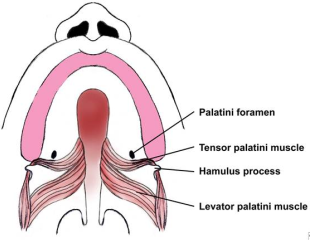
Soft-tissue defects of the cleft palate include hypoplasia of the velar musculature
in addition to anomalous insertions of its muscular components (see the following
image). The normal midline insertion and transverse orientation of the levator palatini
is substituted by an aberrant longitudinal orientation and insertion along the bony
cleft margin and posterior palatine bones. Other palatal muscles are affected similarly.
Dysfunction results in speech pathology with velopharyngeal incompetence and in
eustachian- tube obstruction with resultant middle-ear effusion, infections, and
possible hearing loss.