The following Oropharyngeal deformities are usually associated with the Cleft lip/palate.
Such as: The Robin sequence, macroglossia, ankyloglossia, epignathus, lingual thyroid,
and a few other conditions which are briefly discussed in this section.
Robin Sequence
The Robin sequence includes cleft palate (CP), a small mouth, and retrognathia.
Retrognathism results in a functional abnormality of the tongue musculature that
manifests with airway obstruction during sleep, as the tongue falls posteriorly.
In addition to the respiratory difficulties, feeding difficulties can result in
a failure to thrive.
The severity of airway compromise dictates management. In mild cases, conservative
treatment consists of placing the patient in a prone position and intensive monitoring.
Surgery is indicated if no improvement occurs after 7 days. Surgery involves either
tracheostomy or repositioning of the tongue.
Macroglossia
Congenital macroglossia may be secondary to tumors (eg, dermoids), muscular hypertrophy
or hyperplasia (Beckwith-Wiedemann syndrome), or hemihypertrophy. Vascular malformation
is a common cause of macroglossia. Macroglossia may interfere with speech or
deglutition. In addition, the exposed tongue can become dry, cracked, and ulcerated.
Oral hygiene and drooling can be problematic.
Lymphangiomas are the most common vascular malformations of the tongue. Surgical
biopsy or relatively minor trauma to the patient with lymphangioma can result in
massive swelling, with difficulty in closing the mouth or, at times, airway compromise.
Increased swelling can occur with superimposed lymphangitis. Early in life, conservative
treatment is recommended; this includes the avoidance of trauma and the prompt use
of antibiotics at the first sign of infection. Surgery is usually delayed until
the child is older (4-5 y) to decrease the likelihood of postoperative airway problems.
Macroglossia is a feature of Down syndrome. The etiology is believed to be a reactive
hypertrophy due to muscular hypotonia. The combination of macroglossia and a small
oral cavity in these patients results in glossoptosis. Partial glossectomy is usually
successful in returning the tongue to the oral cavity and in removing this visible
stigma of mental retardation.
Macroglossia can also be associated with a few syndromes, such as Treacher Collins
(mandibulofacial dysostosis or Franceschetti-Zwahlen- Klein) syndrome.
Ankyloglossia
Ankyloglossia is due to the presence of a frenulum tethering the tip of the tongue
to the floor of the mouth. The commonly used term to describe ankyloglossia is tongue-tied.
Problems with articulation may affect sounds that require placement of the tongue
on the upper incisor teeth, as in the /th/ sound. In Spanish-speaking persons with
this condition, rolling of the tongue to produce the /r/ sound is particularly difficult.
Surgical intervention is indicated for articulation problems and for feeding difficulties
(poor suckling), dental problems (spreading of the lower incisor teeth), or requests
by the patient's parents. Release may involve simple division of the involved band
of tissue or a Z-plasty lengthening procedure. Injury to the Wharton duct should
be avoided.
Epignathus
Epignathi are rare teratomas that histologically contain tissue of all 3 germ- cell
lines. Patients usually present at birth with a mass that protrudes through
the mouth and compromises the airway (see the image below). Grossly, the tumor is
covered with skin and mucosa and appears to arise from the palate or pharynx, filling
the oral cavity. These masses are thought to arise from pluripotential stem cells
from the Rathke pouch region.
Prenatal ultrasonography usually demonstrates the mass protruding from the fetal
face. The differential diagnosis should include hairy polyps, encephaloceles, gliomas,
and dermoids.
Management involves emergently securing an airway by intubation or formal tracheostomy.
A magnetic resonance image (MRI) (or computed tomography [CT] scan) is required
before surgical intervention to rule out an encephalocele or intracranial extension
of the lesion. Once the extent of the mass is adequately determined, the tumor can
be excised through the oral cavity.
Lingual Thyroid
A lingual thyroid is due to the undescended thyroid at the tongue base. Common symptoms
include dysphagia; dysphonia; and, occasionally, dyspnea. Thyroid ultrasonography
has replaced radioisotope thyroid scanning in the evaluation of the amount of active
thyroid tissue present.
Management depends on functional and metabolic factors. If the patient is euthyroid,
observation with careful follow-up is advised. Suppressive thyroid hormone therapy
should be initiated if a hypothyroid status develops. If the lingual swelling increases,
surgical excision with replacement therapy is indicated.
Other Conditions
Lip pits represent vestigial remnants of the lateral sulci of the mandible at the
7.5- to 12.5-mm stage of the embryo. In van der Woude syndrome (an autosomal dominant
syndrome with 90% penetrance), lip pits are paramedian and usually bilateral. They
vary in depth from a few millimeters to 3 centimeters or more. A communication may
exist with the minor salivary glands of the lower lip. Lip pits may also occur in
popliteal pterygium syndrome and in aganglionic megacolon with cleft lip and palate
(CLP).
Commissural lip pits occur more frequently than other lip pits and are not related
to the syndromes just described. Their prevalence is estimated to be 1 case per
300 white persons and 1 case per 48 black persons.
Micrognathia could be associated with numerous syndromes and conditions, such as
an adducted thumb, atelosteogenesis (types I and III); cerebrocostomandibular findings;
the Robin sequence; and Aase-Smith, Chitayat-Azouz, chromosome 3 dup 3p, chromosome
4 partial del 4p, chromosome 7 term del 7q, Say, and Shprintzen (velocardiofacial)
syndromes.
Embryology
In facial morphogenesis, neural crest cells migrate into the facial region, where
they form the skeletal and connective tissue and all dental tissues except the enamel.
Vascular endothelium and muscle are of mesodermal origin.
The upper lip is derived from medial nasal and maxillary processes. Failure of merging
between the medial nasal and maxillary processes at 5 weeks' gestation, on one or
both sides, results in cleft lip. Cleft lip usually occurs at the junction between
the central and lateral parts of the upper lip on either side. The cleft may affect
only the upper lip, or it may extend more deeply into the maxilla and the primary
palate. (Cleft of the primary palate includes cleft lip and cleft of the alveolus.)
If the fusion of palatal shelves is impaired also, the cleft lip is accompanied
by cleft palate, forming the cleft lip and palate abnormality.
-
Cleft palate is a partial or total lack of fusion of palatal shelves. It can occur
in numerous ways:
- Defective growth of palatal shelves
- Failure of the shelves to attain a horizontal position
- Lack of contact between shelves
- Rupture after fusion of shelves
The secondary palate develops from the right and left palatal processes. Fusion
of palatal shelves begins at 8 weeks' gestation and continues usually until 12 weeks'
gestation. One hypothesis is that a threshold is noted beyond which delayed movement
of palatal shelves does not allow closure to take place, and this results in a cleft
palate.
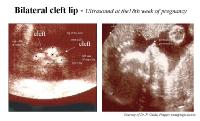
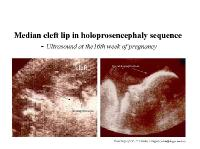
Cleft lip can be easily diagnosed by performing ultrasonography in the second trimester
of pregnancy when the position of the fetal face is located correctly.
Bilateral cleft lip on ultrasound.
Median cleft lip on ultrasound.
Usually, diagnosing a cleft palate with ultrasonography is not possible; however,
an experienced physician or technician may catch an atypical movement of the fetal
tongue in a lateral view. In the case of a large cleft palate, the tongue moves
up into an open space (cleft) in the roof of the oral cavity. Three-dimensional
imaging has been introduced to prenatal ultrasonography diagnostics of cleft anomalies
and appears to be promising for recognizing a cleft palate in a fetus.
Etiology
Generally, facial clefting results when medial, lateral, and maxillary nasal processes
on either left, right or both sides of the forming craniofacial complex do not fuse
completely. Early embryonic changes (during the fourth and tenth weeks of gestation)
may result in clefting. Suspected causes include: 1) environmental insults (i.e.
maternal diseases, chemotherapy, radiation, alcohol, excess retinoic acid and anticonvulsant
medications); or 2) genetic factors.
Researchers have identified some of the genes involved in regulating craniofacial
development. The Human Genome Project hopes to ultimately identify all the genes
that make us human. This should help us to better understand the genetic causes
of cleft lip and palate.
Factors that increase the chance of congenital malformations include: 1) pregnancies
in women older than 35; 2) teenaged pregnancies; and 3) increased consumption of
teratogens during early months of pregnancy (Slavkin 1992).
The good news is that ultrasound, amniocentesis and molecular genetic techniques
can be used to detect common congenital malformations, including cleft lip, early.
Advances in surgical techniques and growth factors also help correct problems associated
with cleft lip or cleft palate. Cleft lip is usually less serious than cleft palate.
A post-pubescent male may choose to grow a mustache to hide the external scar that
remains after childhood surgery has closed the cleft lip. Unfortunately, this easy
cosmetic option is not available to females.
About 22 percent of facial clefting has a genetic origin. Again, most cleft lips
with or without cleft palate are produced by environmental insults (teratogens such
as alcohol, retinoic acid, maternal illness, protein/calorie malnutrition during
pregnancy) interacting with one or more genes. There is increased risk for congenital
malformations because of maternal age at the time of pregnancy.
Additional risk factors include lack of prenatal care during pregnancy, cigarette
smoking, lack of a balanced diet and the chronic use of non- prescribed drugs or
substance abuse. If parents without a cleft have a child with a cleft, the chance
that a subsequent baby will have a cleft is only two to four percent. If either
parent has a cleft, the relative risks become about four to five percent for having
a baby with a cleft. If both parents have clefts, the risks are much greater (Slavkin
1992).
In addition to the required tissue repair, children with cleft lip and palate may
have difficulty hearing or speaking clearly. Thanks to professionals including dentists,
surgeons, and teachers, prognosis is very good. Patients with isolated cleft lip
usually do not have trouble with feeding. However, infants with cleft lip and palate
don't have adequate suction to draw milk through a nipple. Methods have been developed
to enhance maternal bonding during the feeding of newborn and very young infants.